The Norwegian National Network for Arthroplasty and Hip Fractures
The registers continuously collect data from all over Norway on joint replacements, hip fractures, ACL injuries and congenital hip disorders in children.
The Norwegian Arthroplasty Register was established in 1987 by the Norwegian Orthopaedic Association after the use of poor hip prostheses was discovered in the early 1980s. The register was expanded to include all joint replacements in 1994 and was approved as a national medical quality register in 2009.
The Norwegian Knee Ligament Register was established in 2004 and The Norwegian Hip Fracture Register in 2005. Both registrens were approved as national medical quality registers in 2009.
In 2010, the Norwegian Paediatric Hip Register began to record all new cases of hip disorders in children and was approved as a national medical quality register in 2015.
In 2002, the Norwegian Arthroplasty Register was upgraded to a National Advisory Unit by the Ministry of Health and Care Services (HOD). In 2010, HOD changed the Unit’s name to the Norwegian National Advisory Unit on Arthroplasty and Hip Fractures. The name changed again from January 2023 to The Norwegian National Network for Arthroplasty and Hip Fractures.
The Norwegian Paediatric Hip Register began to record paediatric hip dysplasia, Legg-Calvé-Perthes disease (LCPD) and slipped capital femoral epiphysis (SCFE) in 2010 and open and arthroscopic hip surgery (not arthroplasty) in 2013.
The National Network operates the national registers for arthroplasty and hip fractures, and aims to build and disseminate expertise in arthroplasty and hip fractures, in order to enhance the quality and cost effectiveness of treatment.
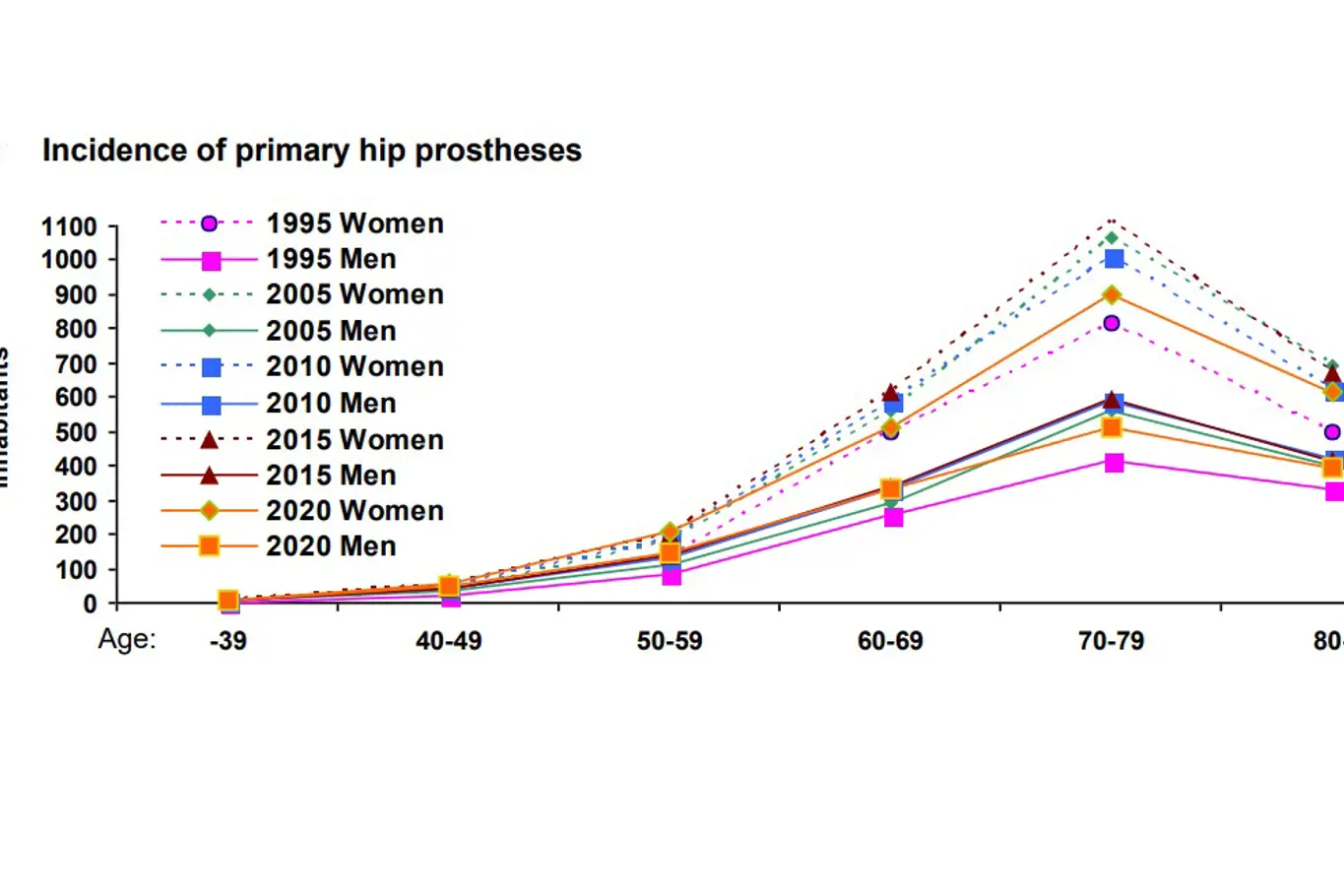
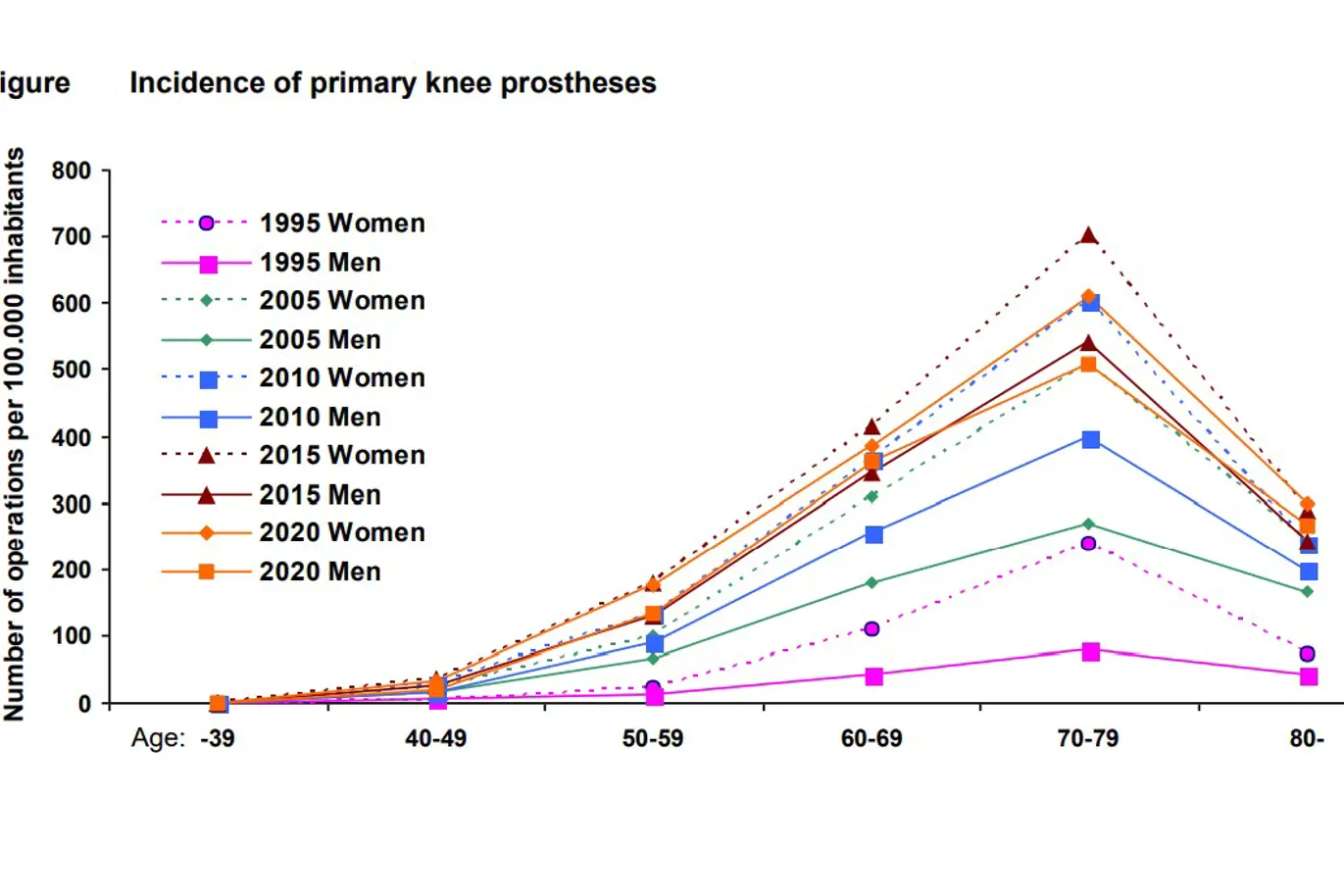
The aim of the registers is to detect poor prostheses, cements and surgical procedures as early as possible and to provide knowledge of epidemiology. With increased expertise in the field and monitoring of the effects of implants and surgical procedures, the quality of treatment is expected to improve. The Advisory Unit also operates the Norwegian Cruciate Ligament Register and the Norwegian Paediatric Hip Register. All registers are initiated by the Norwegian Orthopaedic Association, while the operation of the registers takes place in the Orthopedic Clinic of Haukeland University Hospital, Bergen. Results can be found in our annual report and on the website of the National Service Centre for Medical Quality Registers: www.kvalitetsregistre.no.
The operation of the registers is funded by the health trusts Helse Vest RHF and Helse Bergen HF.
Sist oppdatert 09.04.2024